Open Prostatectomy
Some patients diagnosed with benign prostatic hyperplasia may be recommended to undergo a surgical procedure called an open prostatectomy, or surgery to remove the prostate. The prostate gland is an important organ of the male reproductive system. While the prostate gland of a child is less than the size of a pea, upon reaching the age of twenty, it is like a walnut in shape and size. Around the age of 40, the prostate gland starts to grow in a process called hyperplasia. As the prostate enlarges, the urethra, which passes through the prostate, is squeezed, causing unpleasant physical symptoms, such as frequent urges to urinate, inability to completely empty the bladder, or intermittent urination. These phenomena may be accompanied by pain, involuntary release of urine, or other unpleasant sensations.
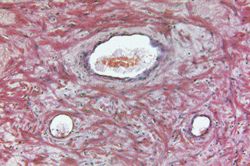
One factor that contributes to the hyperplasia is the increase in the synthesis of an androgen hormone dihydrotestosterone (DHT), which is synthesized primarily in the prostate gland through modification of testosterone, another important male hormone.
If the patient shows symptoms such as an enlarged bladder, changes in the bladder shape or presence of a bladder infection, a urethra obstruction and inability to urinate normally, as well as pathological changes in the kidney and urethra or blood in the urine, then doctors may recommend some type of surgical intervention, including open prostatectomy.
However, open prostatectomy is not recommended to all patients For example, it is not recommended to those, who have previously had surgery on the pelvic organs that makes it difficult to access the prostate; if there is a malignant tumor in the prostate, or if the prostate is not large enough.
In addition to these symptoms of prostatic hyperplasia, one very important factor is the patient's age, since there can be complications related to the age. To establish an accurate diagnosis, it is often necessary for the patient to undergo a series of tests, including ultrasound and blood tests for the presence of a special antigen. If data analysis confirms a suspected tumor, additional procedures, such as a biopsy of the bladder, can be administered. ECG and/or chest X-rays may also be conducted as part of the preoperative stage.
It is important for patients to receive their consultation and examination directly from the surgical specialist, who can evaluate potential risks and side effects. Immediately before the operation, the patient should always consult with the anesthesiologist to discuss possible options during surgery. If the use of general anesthesia is indicated, the anesthesiologist then performs the necessary preliminary assessments and preparations. The most common type of anesthetic for a prostatectomy procedure today, however, is an epidural, which numbs the lower part of the body only, and is associated with far fewer risks (like bleeding).
Two approaches are normally used in open prostatectomy surgery. One of them removes the prostate tissue by making an incision in the tissues of the bladder. An alternative approach is the perineal method, in which prostate tissue removal occurs through an incision in the perineum between the scrotum and the anus.
Modern surgeons use innovative technologies to improve the quality of life for patients after prostatectomy procedures. One effective approach is to preserve the patient's erectile function by saving the relevant nerves.
As a rule, after an open prostatectomy, patients remain in the hospital for 4-7 days. The procedure affects sensitive tissues, and in many cases patients need strong painkillers after surgery. In addition, after this surgery it is necessary to monitor closely and support the bladder function as well as to control fluid balance in the patient's body. A urethral catheter is used to drain the bladder.
A typical patient recovery after an open prostatectomy follows this path:
- For the first 24 hours, the patient is rarely elevated to a sitting position, and they have a liquid diet and soft food that is easy to stomach.
- Over the next 24 hours, the patient is gradually transferred to a regular diet, and if there is no blood in the urine, the urethral catheter can be extracted.
- In the following next 24 hours, the patient s activity increases. After inspecting the surgery area, the surgeon will remove the drainage tube. If there are no complications or additional indications, the patient can be sent home. After about four weeks, the patient returns to his previously normal physical activity.
Thanks to the advanced technology used in this surgery, in most cases it is possible to avoid bleeding. Moreover, doctors can now significantly reduce (up to 3%) the risk of erectile dysfunction. Several other minor side effects, such as temporary incontinence or frequent urges to urinate, may remain for some time after the procedure.
Two out of three patients experience the phenomenon of retrograde ejaculation, but this complication is not considered serious, and does not reduce sexual activity. After an open prostatectomy, though, there is always a risk of serious side effects such as thrombosis, pulmonary embolism, and a stroke, but these occur in less than 1% of all cases.



